Formation of enamel (amelogenesis)
Dental enamel is a complex product of differentiated cell activities of ameloblasts (Fig 3-7). It arises during three processes taking place in the cells simultaneously, namely the formation of enamel matrix, mineralization of the matrix, and maturation of the crystalline structure. Enamel is the mature crystalline framework of prisms (Fig 3-8) and the hardest substance in the human body.
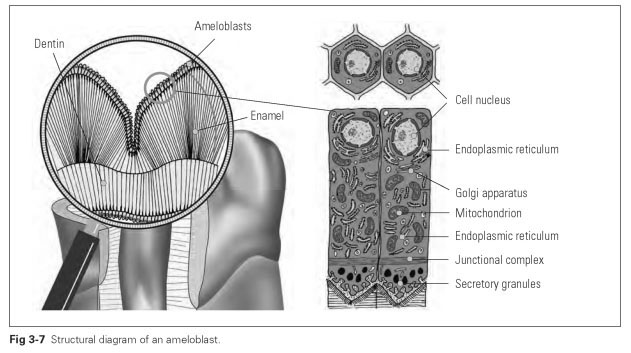
The formation of enamel starts with the secretion of enamel matrix. This secretory process is similar to that of an eccrine glandular cell: In the distinctly enlarged endoplasmic reticulum of the ameloblasts, the proteins of the enamel matrix are synthesized and secreted in an extracellular direction at the distal pole of the cell. The slightly granulated enamel matrix is secreted drop by drop and proliferates. It is made up of protein, carbohydrates, and lipids.
Needle-shaped crystallization seeds of apatite crystals rapidly form in the secreted matrix. The crystallization seeds develop in orderly rows and with gaps, perpendicular to the cell poles of the ameloblasts. The cells control the formation, arrangement, and orientation of the apatite crystals. Enamel prisms develop and lie almost parallel to each other, reflecting the path of ameloblast movement. During the ongoing synthesis of enamel matrix and its mineralization, the am-eloblasts move from the dentinoenamel junction outward just as the enamel prisms lengthen and the enamel thickens. This movement is not linear and centrifugal but happens in growth spurts, as shown by the patterns of lines, the perikymata, visible in the mature enamel.
The mineralization process represents a selective change in the composition of the enamel matrix; when water is removed, the organic parts of the matrix shrink, and calcium phosphate salts are laid down.These rebuilding processes are the cellular activities of the ameloblasts. The preemptive maturation of enamel denotes the processes in which the mineralized enamel matrix becomes the crystalline structure of enamel. The mineralized enamel matrix initially contains about 25% crystalline components, whereas crystals account for 86% of the volume in mature enamel (see Fig 3-6).
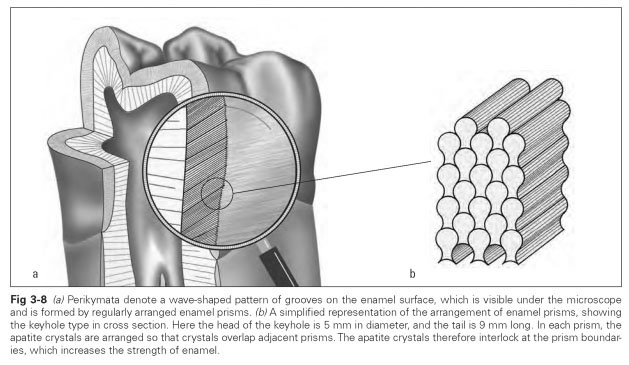
The prisms in mature enamel are made up of apatite crystals of calcium phosphate in the form of hexagonal rods about 0.016 mm long. An organic matrix is stored in the crystals, occupying about 2% of the volume (see Fig 3-6). The interfaces between individual prisms can be seen because the crystals with different growth directions collide with each other. No interprismatic filler material that differs from prisms in its chemical composition can be detected. The number of prisms per square millimeter varies from around 20,000 to 30,000 from the crown to the root, while the number of ameloblasts remains equally high. The enamel prisms stop immediately before the enamel surface; the top layer itself is prism-free. The enamel layer regularly found in unerupted teeth is harder, chemically more resistant, and withstands caries far longer than the rest of the enamel. Large amounts of fluoride are stored in this layer.
The formation of hard substance starts at the tips of the cusps or incisally at the cutting edges and spreads in a labiolingual and mesiodistal direction throughout the crown of the tooth. In the process, the ameloblast layer of the enamel organ moves outward, and the odontoblast layer shifts inward, narrowing the dental papilla on the one hand and the stellate reticulum on the other.
For multicusped teeth, the formation of enamel starts at the various tips of the cusps simultaneously. Once these enamel caps join up, a valley is formed between the enamel ridges. Amelo-blasts become compressed in the bottom of this valley so that the valley walls move closer and closer together. This produces the fissures found in teeth with grinding surfaces. Fissure depth and width as well as the density of enamel under the fissures differ considerably within the individual teeth.
After eruption, the enamel substance then undergoes changes, a process referred to as post-eruptive enamel maturation. During this process, the enamel loses more and more water and organic matrix components. The crystalline structure becomes denser and changes its chemical composition mainly through substitution of hydroxide (OH) groups with fluoride. The enamel becomes even harder and more chemically resistant but more brittle and less permeable. Now the enamel is also more susceptible to fracture, and microcracks appear. When filled with saliva, these microcracks cause discoloration in the form of enamel crack lines. The surface of the enamel also changes as a result of abrasion during chewing and cleaning of the teeth. The enamel layer may be entirely worn away in places, resulting in exposure of the dentin. The dentin layer thus brought to the surface becomes more mineralized by the ongoing activity of the dentin-forming cells (odontoblasts) and is then denser and harder than normal dentin.
As a result of the aging processes, enamel changes from transparent to a gray base color. Ingredients of medicines can lodge in the crystals of enamel, forming solid calcium compounds and staining the tooth a brownish or yellowish color.
Topical fluoridation of the enamel, as a caries-preventive measure, builds up a high concentration of fluoride at the enamel surface. Fluoride solutions are applied so that fluoride ions diffuse into the surface, achieving through substitution of the OH groups a stable, crystalline fluoride compound with the apatites, which protects the enamel against attack from caries. Acidic inorganic fluorides (eg, sodium fluoride, phosphate fluoride) are water-soluble and are washed out within a short time. Organic aminofluorides are not washed out and are better suited to fluoridation of the enamel surface.
During eruption, the ameloblasts are resorbed, transform into squamous epithelium, and lose their ability to divide.They migrate to the gingival sulcus and sustain the enamel-mucosa epithelial attachment during eruption, after which they are shed. Whether the enamel cuticle is made up of transformed ameloblasts cannot be said with certainty. The highly resistant enamel surface is the prism-free layer of enamel. Dentin and enamel are formed layer by layer, as shown clearly by the growth lines (including perikymata).
The root develops from what is known as the Hertwig epithelial root sheath. This is the area of the cervical loop where the internal and external enamel epithelia cross each other. When enamel growth has reached the future cementoenamel junction, the cervical loop lengthens considerably. Hertwig epithelial root sheath determines the ultimate shape, size, and number of roots. The roots differentiate during eruption; while the crown is raised up from the jaw by the primary fibers of the periodontal ligament, the roots grow down in the same way and mechanically support the eruption of the teeth by exerting growth pressure.